In a landmark study of 125 Australian children with high-risk cancer—whose tumour cells were grown in the lab and tested against a suite of potential therapies—Children’s Cancer Institute researchers have found that they can improve the chances of finding the right drug to kill their individual cancer through a new system of rapid drug screening.
The children are enrolled in the ZERO Childhood Cancer Program (ZERO), a world-leading precision medicine program led by Children’s Cancer Institute and Kids Cancer Centre at Sydney Children’s Hospital, Randwick, together with all eight of Australia’s children’s hospitals. In this study—published in the high-impact journal Cancer Research, a journal of the American Association for Cancer Research—Children’s Cancer Institute scientists, led by Senior Scientist in the Personalised Medicine theme Dr Emmy Dolman, took the personalised medicine approach that is the hallmark of ZERO, by incorporating an additional step in the testing of patient samples, known as ‘high-throughput drug screening’.
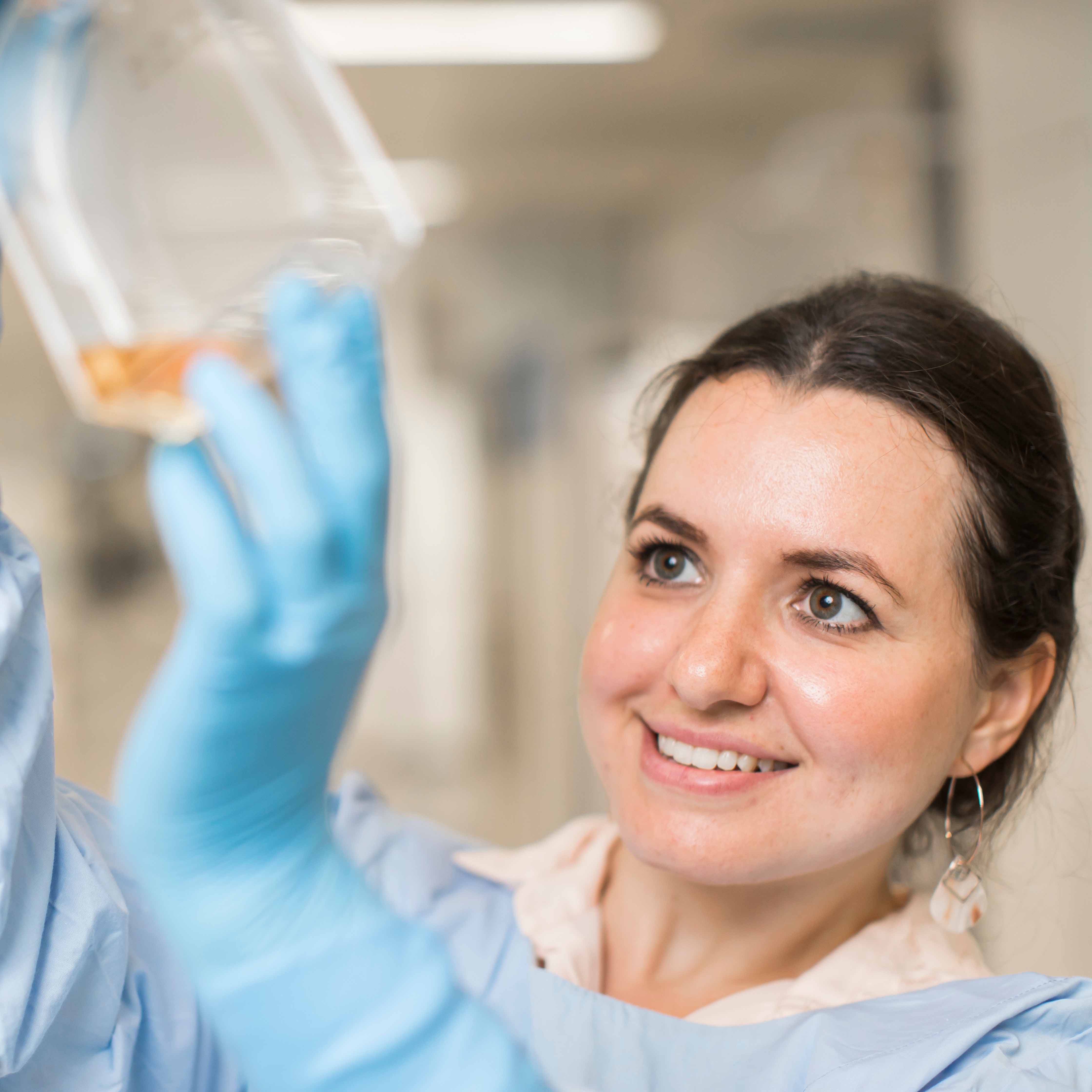
High-throughput drug screening involves growing cancer cells from a patient’s primary tumour sample in the laboratory, then screening these cells against potential drug treatments to see how the cancer responds. Once drugs that have the potential to kill an individual child’s cancer are isolated, these are tested inpatient-derived tumour models of the cancer to further validate their potential efficacy.
According to Dr Dolman, senior author on the published paper, current personalised medicine provides tailored treatment for each individual patient based on patient-specific factors such as genetics. However, for one third of paediatric cancer patients enrolled in these programs genetic profiling alone does not yield a therapy.
“Precision medicine is still an evolving field, and it is not currently possible to identify the right treatment for every child with cancer,” said Dr Dolman. “This new research is an important step towards achieving that goal.”
Past results from ZERO have shown that genomic analysis (genetic testing) of patient samples can reveal the genetic causes of cancer in more than 94 per cent of children with high-risk cancers. Genomic analysis in these children leads to treatment recommendations in about 70 per cent of cases, leaving a gap of about 30 per cent.
“Genomic analysis, which includes whole genome sequencing and RNA sequencing, does not always provide enough information to lead to a treatment recommendation for every child with cancer,” explained Dr Dolman. “Even when we do find a change in the genes in a cancer cell that might be targeted with a specific therapy, that does not always mean it will work.”
“Adding high-throughput drug screening is one way of testing a drug or drug combination to see how effective it might be.”
A pilot trial of high-throughput drug screening, published by Children’s Cancer Institute scientists in 2021, was the first study in the world to demonstrate that this type of screening could significantly improve the identification of treatment options for children with high-risk cancer, revealing additional drug sensitivities and proving a good predictor of clinical response in patients.
The current study confirmed the value of incorporating drug screening into precision medicine programs to support clinical decision making. But more than this, it provided important new evidence of its potential to improve our understanding of children’s cancers and how best to treat them.
“What we learned in our study is that adding drug screening to genomic analysis can help us better understand drug responses. That is, it can help us understand why a particular cancer responds the way it does to a particular drug,” explained Dr Dolman. “And as we learn more, we will be better able to predict which patients are likely to benefit from which therapies.”
Dr Dolman is also excited about the potential for high-throughput drug screening to provide new insights into the biology of children’s cancer.
“When genome sequencing is done on a child’s cancer cells, sometimes it doesn’t reveal a known target for therapy or how the genomic changes we observe are really driving the cancer.
“If we then do drug screening on those cells, and they respond to a certain drug, this gives us important clues about how the genomic changes we have seen are working to drive the cancer’s growth. This could help us identify new biomarkers that indicate which cancers might respond to which drugs. Ultimately, we hope this leads to better ways to select the right drugs for the right patients.”
Another important finding of the study was that screening cancer cells against individual drugs, then correlating the sensitivity profiles of those individual drugs, allowed for the prediction of effective combinations of treatment drugs.
“Treatment with single agents is often not enough to cure cancer, so identifying potential drug combinations is crucial to improving therapeutic options and clinical outcomes for children with cancer,” said Dr Dolman.
Media contact:
Tania Ewing
0408 378 422
taniaewing@taniaewing.com