May is Brain Cancer Awareness month – a time for learning more about brain cancer and helping raise awareness of its impact. And this year, we have some very positive news about developments that are set to impact all Australian kids diagnosed with this disease.
Personalised medicine for cancer
‘Personalised medicine’ means tailoring treatment to suit each individual patient. Two children who have the same type of cancer (medulloblastoma, for example) may show the same symptoms but respond quite differently to the same treatment. That’s because every child is unique, and so too is every child’s cancer. This is why treatment needs to be tailored to the individual.
A similar term that scientists and doctors often use instead of personalised medicine is ‘precision medicine’. This refers to medicine, or patient care, which is based on the factors that make each of us unique, especially our genetics. For example, a person found to have a cancer with a certain gene mutation (alteration) may be treated with a drug known to specifically target that alteration.
The Zero Childhood Cancer Program
Currently, children with aggressive brain cancers in hospitals right around Australia are gaining access to precision medicine through the Zero Childhood Cancer Program (ZERO) − Australia’s first-ever personalised medicine program for children with cancer, jointly led by our Institute and the Kids Cancer Centre at Sydney Children’s Hospital, Randwick. As of May 2022, over 700 children with high-risk brain tumours have been enrolled on the ZERO national clinical trial, which has been running since 2017.
Building on its successes to date, and supported by government and philanthropic funding, ZERO is now being progressively expanded. By the end of 2023, all children and young people (0-25 years) who are diagnosed with cancer in Australia will be able to join the Program.
Brain cancer a top priority
The first stage of ZERO’s expansion will focus on brain cancers. This means that every Australian child with brain cancer, regardless of their prognosis, will have access to personalised medicine – something that has never before been possible.
This expansion may not only benefit children who join ZERO, but will also vastly expand our capacity to carry out brain cancer research in the lab, benefiting other children in the future. This is because every child who participates in ZERO provides samples that are sent for molecular analysis (tumour profiling), and every time a sample is analysed, more data is obtained. These samples and data are creating an incredible resource for scientists and fuelling a whole range of new research projects.

Brain cancer research and ZERO
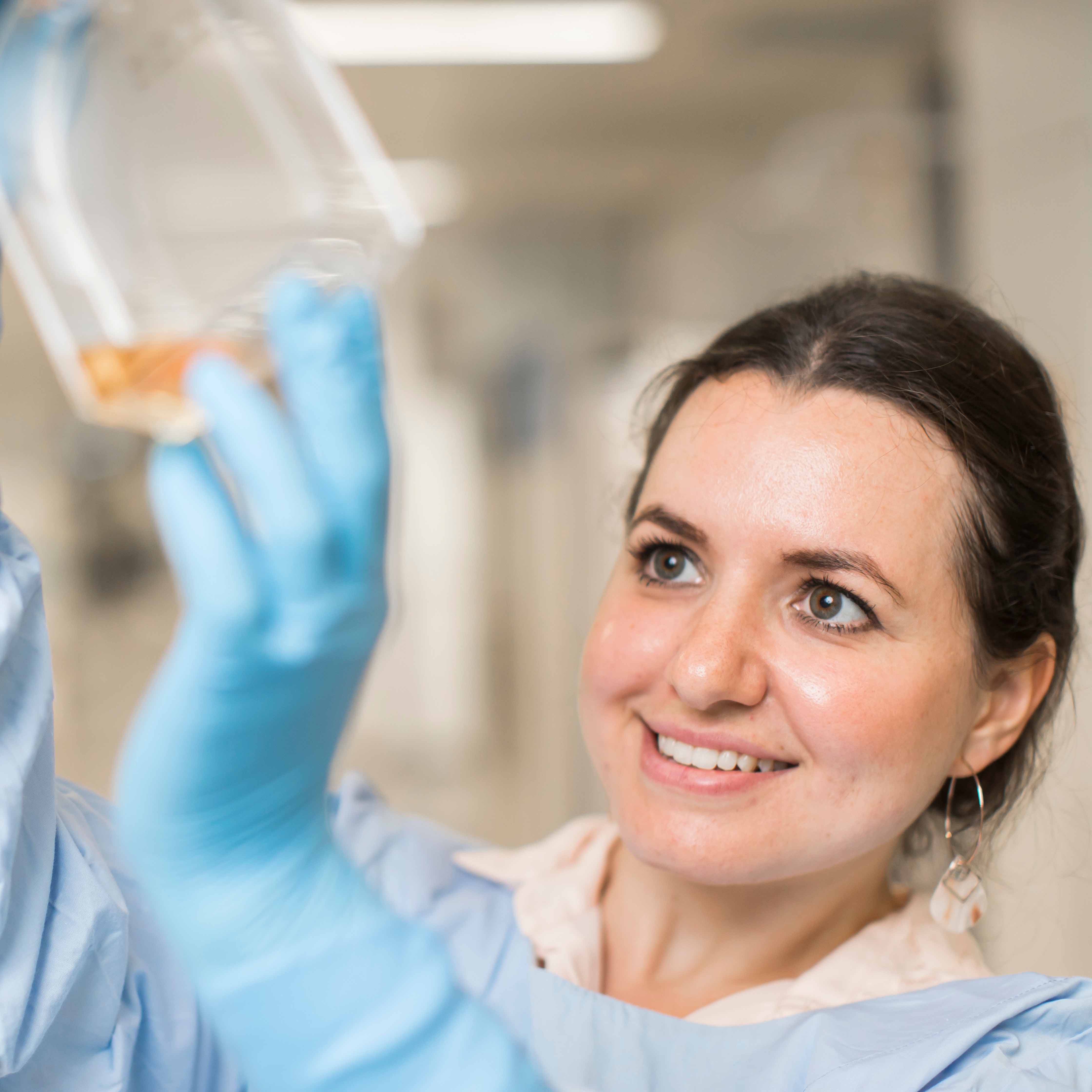
Since the ZERO national clinical trial began, our brain cancer researchers have been able to make important progress in the lab. Using patient samples, we’ve been able to establish more than 40 primary cell cultures for several brain cancers (including glioblastoma, medulloblastoma, DIPG and ependymoma) and have developed living laboratory models of these cancers, called patient-derived xenografts.
These ‘preclinical models’, as they are known, are precious laboratory tools. Many are unique for their molecular alterations and, in some cases, are the only one of their kind in the world. In a laboratory setting, these models represent patients with cancer, and allow us to test new treatments for their effectiveness against particular cancers.
We’ve also been able to develop a panel of healthy brain cells, such as astrocytes and microglia. These are extremely rare and represent perfect controls for childhood brain tumours in experimental work, such as immunotherapy research.
Where ZERO is taking us
ZERO is taking us to an exciting new world of personalised medicine – a world where every child with brain cancer is recognised and treated as unique. Where clinicians have access to unprecedented information about each patient’s cancer, and are able to use this information to help guide diagnosis, prognosis, risk stratification and treatment.
From a research perspective, the analysis of samples from every child with brain cancer is providing access to a wealth of data that simply hasn’t been available before. Scientists have a unique opportunity to identify new molecular targets (molecules responsible for driving the growth of certain cancers), develop new targeted therapies, and test these therapies in newly established preclinical models. We will also learn more about how brain tumours progress over time, how they develop anticancer drug resistance, and if it’s possible to counteract that resistance.
Excitingly, the resources gathered through ZERO will ultimately lead to the establishment of an Australian paediatric brain tumour bank. Here, biological samples from children with brain cancer will be linked with unique genomic and clinical data, providing an incredibly valuable source of information and fuelling cancer research not only throughout Australia, but worldwide.