July is Sarcoma Awareness month – a time for learning more about sarcoma and its impact. In this blog, we introduce an exciting new research project investigating the potential use of immunotherapy to help children with sarcoma.
Sarcoma in children
Sarcomas are tumours of the bones, cartilage and other connective tissues. Because these tumours tend to grow very aggressively, they often require intensive treatment, including highly toxic chemotherapy. Not only does such intensive therapy often result in serious side-effects, it is by no means guaranteed to be effective.
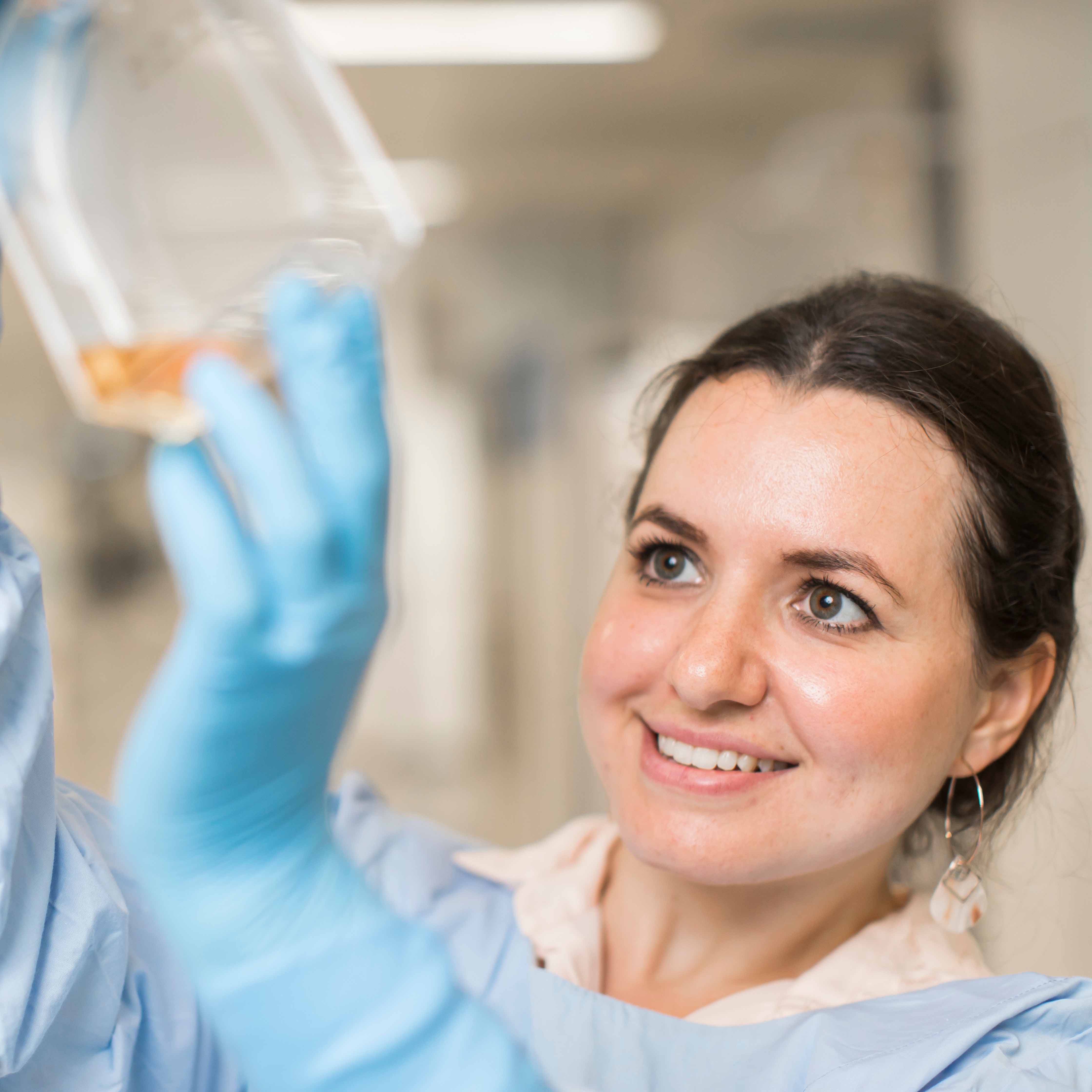
“While cure rates for some childhood cancers such as leukaemia have gone up significantly over the years, cure rates for most types of sarcoma have stagnated,” explains Dr Klaartje Somers, Senior Scientist in our Molecular Targets and Cancer Therapeutics Theme.
“Too many children with sarcoma are dying, and those who survive are often left with serious health issues as a result of their treatment. We desperately need new treatment strategies for these kids.”
Why immunotherapy?
Some years back, it was discovered that our immune system − our body’s natural defence system against disease-causing organisms like bacteria and viruses − is capable of targeting cancer cells. Since then, scientists have been trying to find a way to harness the immune system to fight cancer.
“Using immunotherapy, we can make treatment much more specific to cancer cells, and because of this, less damage is done to healthy cells,” explains Klaartje. “So first and foremost, immunotherapy promises to be much safer than chemotherapy. It could also prove to be a useful alternative treatment in cases where a child’s cancer has become resistant to chemotherapy.”
CAR-T cell therapy
Recently, Klaartje was successful in attracting major Cancer Council NSW funding to support her research into immunotherapy for solid tumours in children. Specifically, she is working on a type of immunotherapy known as ‘CAR-T cell therapy’.
In CAR-T cell therapy, specialised immune cells called T cells are taken from the patient’s blood (or that of a donor) and engineered in the lab, so they are able to recognise and destroy cancer cells when put in the patient’s body. The letters ‘CAR’ stand for chimeric antigen receptor, and reflect the type of receptor the modified T cells express so they can target the cancer cells.
Overcoming obstacles
“CAR-T-cell therapy is one of the most commonly used immunotherapies in kids, but so far it’s been exclusively used for the treatment of blood cancers,” explains Klaartje.
“At the moment, CAR-T cells don’t work well with solid tumours. This is partly because they can’t penetrate the cancerous tissue, and partly because these tumours tend to be quite immunosuppressive, and that’s due to the nature of the tumour microenvironment, or TME [the cells surrounding the tumour].”
Klaartje and her team are working on overcoming those barriers by using special drugs to prime the TME − putting the cancer cells under stress and helping make the tumour more permissive for CAR-T cells to enter − before injecting the cells.
“This is the first time that these drugs have been used for this purpose, to the best of my knowledge,” she shares. “We have a few different drugs to work with, so I’m optimistic about the results we can achieve.”
The team is working closely with Dr Deborah Meyran and colleagues at the Peter MacCallum Cancer Centre to generate CAR-T cells that have been specifically designed to target cancers in children, rather than adults.
Making progress
Recently, Klaartje and her team were able to show that their new technique of using primer drugs to rewire the TME can successfully change the TME in neuroblastoma tumours. Now, they are working on using the same technique with sarcomas.
After working out optimal drug doses and time points for administration, they then plan to test their approach in living models of cancer – mice that have been specially bred for such experiments – to find out if the immunotherapy is more effective and better tolerated than standard therapy.
Looking to the future, Klaartje says she has high hopes about what this research can achieve. “I would love to see this new generation of CAR-T cells move into the clinic and make a real difference for kids with sarcoma and other high-risk solid tumours.”
“It might even be that immunotherapy becomes a first-line therapy in the future, taking the place of chemotherapy. That would be amazing!”
To find out more visit: https://ccia.support/Immunotherapy