Diffuse Intrinsic Pontine Glioma (DIPG) is a brain cancer considered the most aggressive and devastating of all paediatric tumours, and represents 10-15% of paediatric tumours of the central nervous system. DIPG is a highly malignant cancer that arises in early childhood in the brainstem, the most critical part of the brain. Due to its sensitive location, surgery and even biopsy isn’t possible. Patients don’t respond to chemotherapy, and radiation therapy only briefly delays tumour progression. So the outlook for children with DIPG is very poor. Effective treatment options are desperately needed. But because DIPG is rare compared to other childhood cancers and especially adult cancers, medical research funding is difficult to source.
Our research
Our Targeted Therapy laboratory, headed by researcher-clinician Dr David Ziegler, focusses on developing innovative therapies for the most aggressive childhood cancers with a goal of rapid translation to the clinic. A key area of research is investigating new treatment strategies for DIPG and other malignant childhood brain tumours.
A critical problem in improving treatments has been the lack of surgical tissue for biological studies in the laboratory. To solve this, we’ve initiated a national DIPG tumour donation protocol. This, for the first time, allows us to collect tumour samples in rare cases that a biopsy is performed, and allows parents to donate their child’s tumour for research after a child has died. This has allowed us to establish the only laboratory program in Australia dedicated to DIPG research and finding new treatments for this deadly disease. The study owes its existence to the incredible generosity of parents wanting to help other families.

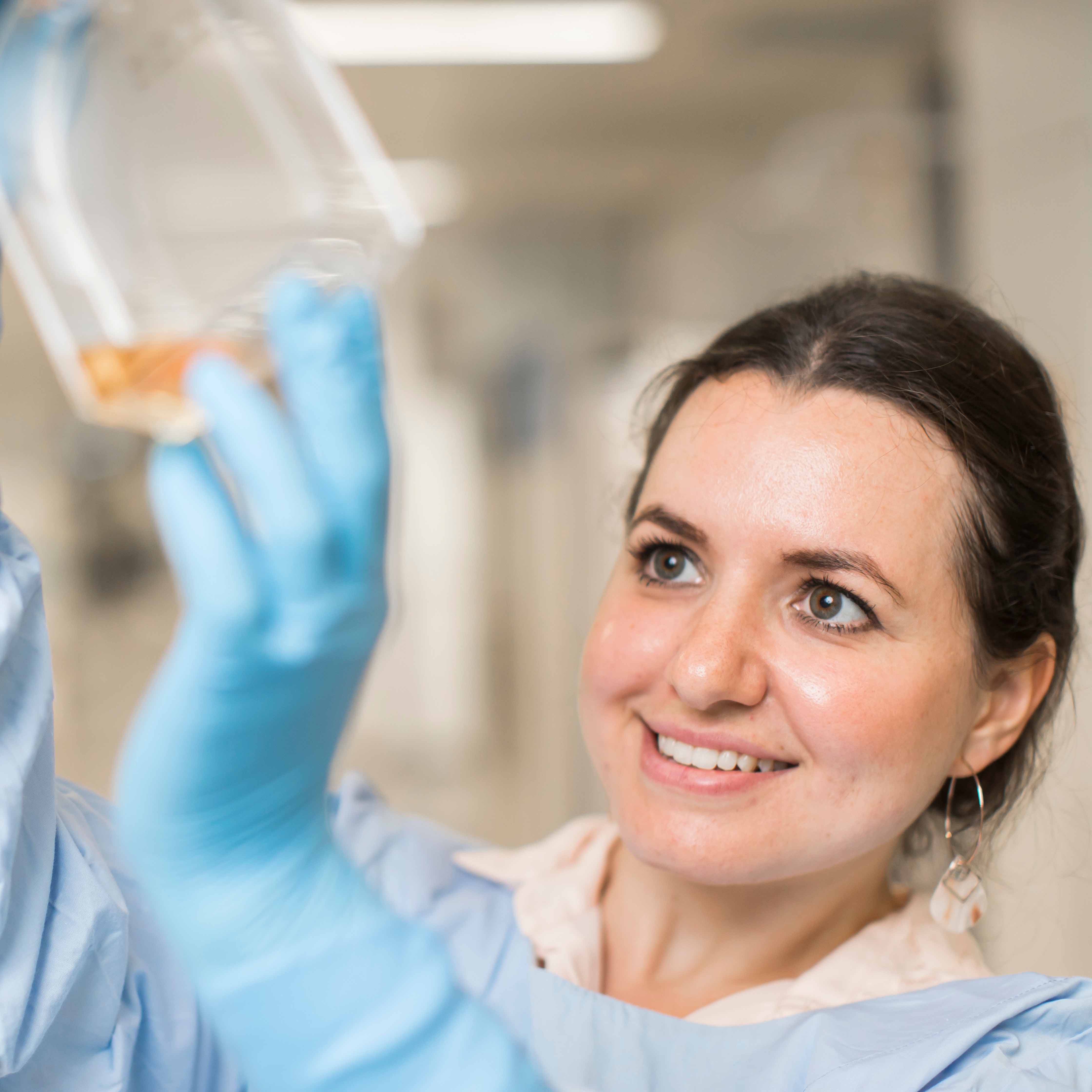
With tissue donated from autopsies we’ve grown a panel of DIPG neurosphere cultures, cancer cells in 3D – a unique way to investigate DIPG’s biology and test new therapies. In the past three years, we’ve screened 3,700 pharmaceutical compounds and found some very exciting potential new treatments. Further screens have identified potentially useful combination therapies to explore further. Our ultimate aim? To develop the most potent anti-DIPG therapies to rapidly translate to the clinic.
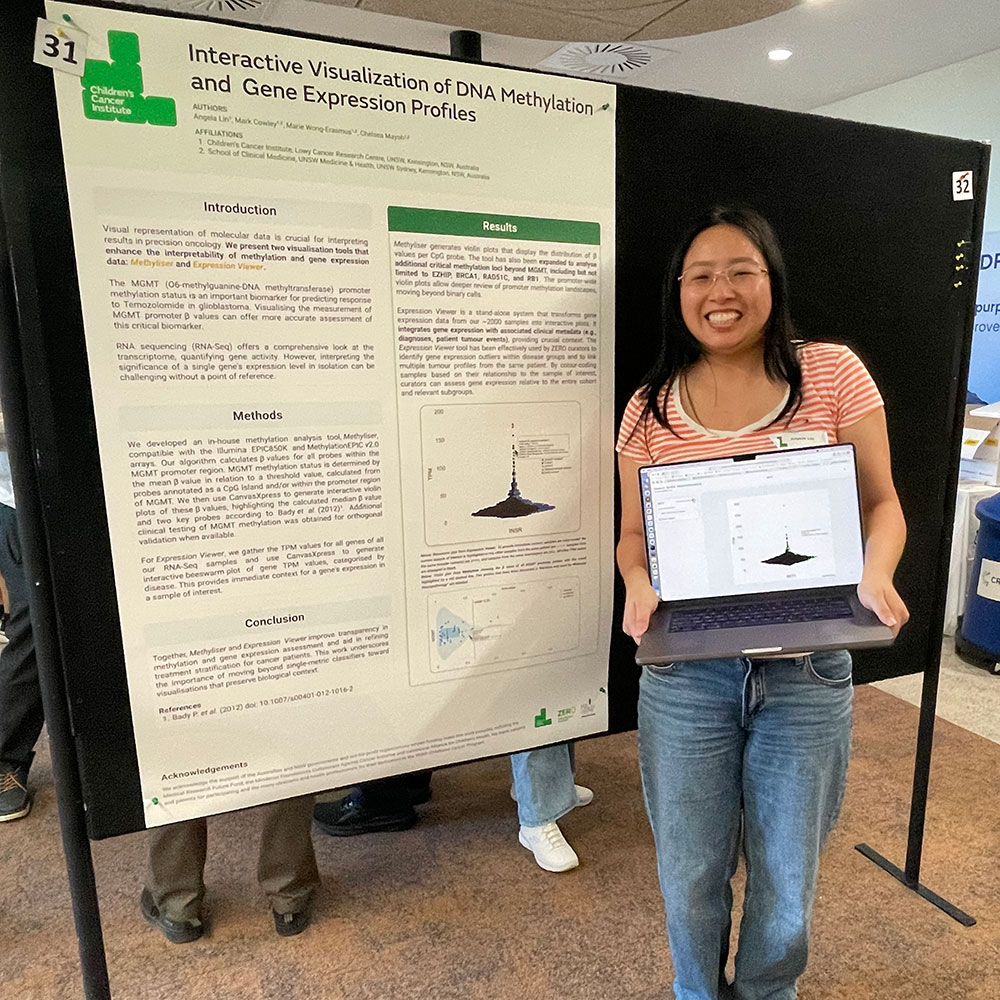
Our research also focusses on developing individualised treatment for all children with high risk brain tumours. We’re spearheading a national clinical trial as part of the Zero Childhood Cancer national personalised medicine program. A flagship initiative of Children’s Cancer Institute and the Sydney Children’s Hospital, it’s in pilot stage. Children with brain tumours make up half of all patients in this study because of the need to find better treatments. We comprehensively assess every brain tumour – analysing the tumour’s genetic landscape, testing the activity of different drugs in the test tube, and developing individualised mouse models for each child. We’ve made several exciting discoveries, and identified new treatment options for specific children with different brain tumour types. Ultimately, we aim to transform the way every child with a high risk brain tumour in Australia is diagnosed and treated.
Meet a researcher

Our Targeted Therapies lab in Sydney is a long way from the small town in Greece where Senior Research Officer Dr Maria Tsoli grew up. After studying and working in Australia, Germany and the US, Maria now works in DIPG research at Children’s Cancer Institute. Read more in our new issue of LabNotes newsletter for Spring 2016 (pdf, 0.7MB).